 Tick-Borne Encephalitis
Tick-Borne Encephalitis
 What is it?
What is it?
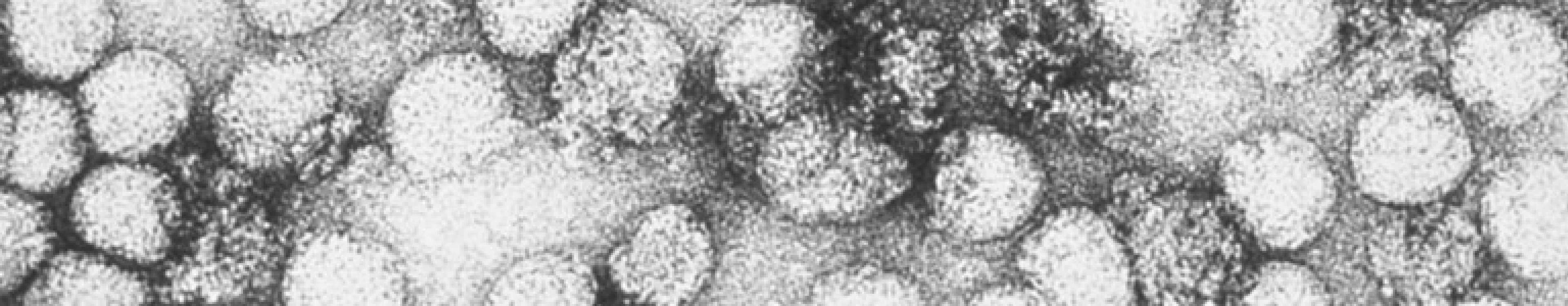
Tick-borne encephalitis (TBE) is a viral infection that affects the central nervous system (brain and spinal cord) causing a spectrum of disease ranging from a mild illness to a more severe, life-threatening illness. It is usually transmitted through the bite of an infected tick.
 Who is at risk?
Who is at risk?
TBE is common in an area that extends from Central, Eastern and Northern Europe across Russia to parts of East Asia. There are five subtypes of TBE virus, the three main types are:
- European – common in Europe and western Russia
- Siberian – common in Russia and parts of eastern Europe and northern Asia
- Far Eastern – common in eastern Russia, China and Japan
It is a rare disease, but people are at increased risk if they visit woodland or grassland in high-risk areas for example when camping or hiking.
 What are the symptoms?
What are the symptoms?
Many people with TBE have no symptoms, but between 2–30% of infected people develop a temperature after about 8 days. TBE typically occurs in two stages. The first is a mild flu-like illness and while many people recover after this stage, about a third of the people with these symptoms go on to develop the second stage of the illness. The second stage is more severe, and many of these people will go on to have long-term complications. It is rarely fatal in Europe, however in Asia it may be fatal in up to 20% of cases.
 How is it spread?
How is it spread?
Tick-borne encephalitis is usually transmitted through the bite of an infected tick,or less commonly through the ingestion of unpasteurised milk. Ticks can live on mice, voles, sheep, goats, cattle and some species of birds. Ticks are found on the edge of forests in grassland, forest glades, riverside meadows and marshland, forest plantations with brushwood and shrubbery. People who are camping or hiking in high-risk areas may be at risk of being bitten by an infected tick. People can also be infected by eating or drinking unpasteurised dairy products.
 How can it be prevented?
How can it be prevented?
Avoid known heavily tick-infested areas of forest and woodland during the spring, summer and autumn where possible. Check your body for ticks regularly. Common areas for ticks to attach are at the hair-line, elbows, backs of knees, groin and armpits. You should also avoid unpasteurised dairy products in high-risk areas.
A vaccine is available that can help protect against TBE. You may be advised to consider vaccination depending on where you are travelling to and your planned activities.
 How can it be treated?
How can it be treated?
There is no specific anti-viral treatment for tick-borne encephalitis. More severely affected people may need to be treated in intensive care and some may require assistance with breathing. Long-term support for neurological complications also may be needed.
 Where can I get further information?
Where can I get further information?
If you have any questions or concerns about exposure to tick-borne encephalitis, please speak to your doctor or a travel health practitioner for more information.
Make sure you contact your GP or travel health practitioner in plenty of time before you travel to discuss the ways you can help to keep yourself healthy whilst away. You should try and contact them at least 4–6 weeks before your trip.
After your trip, you should contact your GP if you develop a fever or notice any other unusual symptoms.
The information provided is a summary that was up to date when this article was published; however, recommendations may be updated from time to time. Please always consult with your doctor, nurse or pharmacist well in advance of travelling.
References
1. Travel Health Pro. Tick-borne encephalitis. Available at: https://travelhealthpro.org.uk/factsheet/22/tick-borne-encephalitis. Accessed February 2024.
MAT-XU-2203069(v2.0) | February 2024
For further information please talk to your healthcare professional

